
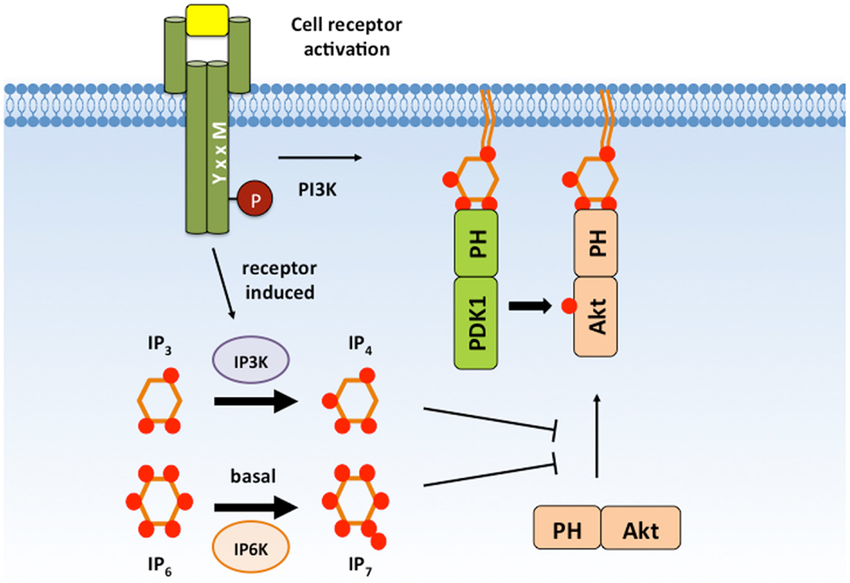
IVIG significantly attenuated the ICH-induced increase of brain water content in ipsilateral basal BBB at 24 ( a) and shown the strong tendency to improvement at 72 hours ( b) after ICH. ICH increased water content in brain of ICH- compared to sham-operated animals evaluated at 24 ( a) and 72 hours ( b) after ICH. IVIG attenuated BBB disruption after ICH without affecting the hematoma volume. We conclude that IVIG treatment represents a promising therapeutic approach potentially able to decrease mortality and morbidity after ICH in experimental models. Furthermore using siRNA-induced in vivo knockdown approach we demonstrated that beneficial effects of IVIG were mediated, at least partly, via SHIP1/PIP3 pathway. Mast cell deactivation resulted in reduced inflammation, consequently attenuating brain edema and improving of neurological functions after ICH. We demonstrated that while ICH induced mast cell activation/degranulation, IVIG attenuated post-ICH mast cell activation. To prove this hypothesis we employed the ICH collagenase mouse model. We hypothesized that IVIG will attenuate the ICH-induced mast cell activation via FcγRIIB/SHIP1 pathway, resulting in a decrease of brain inflammation, protection of the blood-brain-barrier, and improvement of neurological functions after ICH. Intravenous immunoglobulin (IVIG) is a FDA-approved drug containing IgG. It's signals are mediated by SHIP (Src homology 2-containing inositol 5' phosphatase), in particular SHIP1, which activation leads to hydrolyzation of PIP3 (Phosphatidylinositol (3,4,5)-trisphosphate (PtdIns(3,4,5)P 3, leading to the inhibition of calcium mobilization and to the attenuation of mast cell activation. The mast cell activation is negatively regulated by an inhibitory IgG-receptor. Following intracerebral hemorrhage (ICH), the activation of mast cell contributes to brain inflammation and brain injury.


 0 kommentar(er)
0 kommentar(er)
